Disclaimer: Early release articles are not considered as final versions. Any changes will be reflected in the online version in the month the article is officially released.
Author affiliation: Liverpool School of Tropical Medicine, Liverpool, UK (A.M. O’Ferrall, S.A. Kayuni, L.J. Cunningham, J. Archer, A.P. Roberts, J.R. Stothard); Malawi-Liverpool-Wellcome Trust Clinical Research Programme, Queen Elizabeth Central Hospital, Blantyre, Malawi (S.A. Kayuni, P. Makaula, J. Musaya); School of Medicine and Oral Health, Kamuzu University of Health Sciences, Blantyre (S.A. Kayuni, J. Musaya); Wolfson Wellcome Biomedical Laboratories, Natural History Museum, London, UK (J. Archer)
Schistosomiasis is a waterborne, parasitic disease transmitted by several species of Bulinus and Biomphalaria, two distinct freshwater snail genera common across sub-Saharan Africa (1). In sub-Saharan Africa, Schistosoma haematobium is the predominant cause of urogenital schistosomiasis, and S. mansoni is the predominant cause of intestinal schistosomiasis (1). S. haematobium is endemic in Malawi, where infections with zoonotic and hybrid species from the S. haematobium group (S. mattheei and S. haematobium × S. mattheei) have also been detected in humans (2,3). S. mattheei is considered a livestock-infecting schistosome that causes intestinal disease (4); however, excretion of ova from humans infected with S. mattheei and associated S. haematobium group hybrids reportedly has occurred through the urogenital tract (2,3). Meanwhile, Biomphalaria freshwater snails were first detected along the southern shores of Lake Malawi in 2017 (5). Since then, autochthonous S. mansoni transmission and intestinal schistosomiasis outbreaks have been confirmed in Mangochi District, Malawi (5,6).
To clarify S. haematobium group hybridization dynamics, we conducted a longitudinal cohort study in southern Malawi. The College of Medicine Research Ethics Committee, Malawi (approval no. P.08/21/3381, https://www.ncst.mw) and the Liverpool School of Tropical Medicine Research Ethics Committee, United Kingdom (approval no. 22-028, https://www.lstmed.ac.uk/research/research-integrity/research-ethics-committee) provided ethics approval. This study also tracked S. mansoni prevalence in a community cohort recruited from Samama Village, Mangochi District (Appendix Figure 1), where the outbreak of intestinal schistosomiasis was initially reported (5,6).
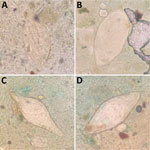
In June 2024, we determined S. mansoni prevalence in Mangochi District to be 14.8% (165/1,116) using point-of-care urine circulating cathodic antigen cassette tests (POC-CCA; ICT International, https://ictinternational.com), and considered trace results positive. Those results represented the lowest reported S. mansoni prevalence in Samama Village since it emerged in 2017 (5–7). However, we observed numerous atypical schistosome ova within feces provided by 2 POC-CCA–positive participants upon Kato-Katz examination (https://microbeonline.com/kato-katz-technique-principle-procedure-results) (Figure). Patient X, a 10-year-old girl, and patient Y, a 19-year-old man (Table), both received treatment with praziquantel from a study-affiliated clinician. The unexpected morphologic diversity raised concerns about underreporting of intestinal schistosomiasis being caused by species other than S. mansoni, prompting closer molecular analysis for robust speciation that cannot be achieved by microscopy.
We obtained hatched miracidia from the urine and feces of patients X and Y by using Pitchford-Visser filtration and collected and preserved individual miracidia on Whatman Flinders Technology Associates cards (GE Healthcare Life Sciences, https://www.gehealthcare.com/products/life-sciences), according to standard protocols (8). To identify the schistosome larvae, we used a newly described 2-tube high-resolution melt real-time PCR assay on DNA extracted from individual preserved miracidia (9). To detect evidence of mixed ancestry or putative genetic introgression, we targeted both the nuclear DNA ribosomal internal transcribed spacer 2 locus and species-specific mitochondrial DNA (mtDNA) loci of 6 Schistosoma species: S. bovis, S. curassoni, S. haematobium, S. mansoni, S. margrebowiei, and S. mattheei. For S. bovis, S. curassoni, S. haematobium, and S. mansoni we targeted the tRNA lysine region; for S. margrebowiei the NADH dehydrogenase subunit 4 region; and for S. mattheei, the NADH dehydrogenase subunit 6 region.
Miracidia hatched from ova in the feces of patient X mostly typed as S. haematobium × S. mattheei hybrids (93.3%), whereas most miracidia hatched from the paired urine sample typed as pure S. haematobium (95.8%). Similarly, atypical zoonotic and hybrid schistosome species ova from patient Y were predominantly in feces (Appendix Figure 2). Of the 59 S. haematobium × S. mattheei hybrid miracidia typed from feces, high-resolution melt profiles indicated that mtDNA (maternal) was inherited from S. mattheei in 58 miracidia, although S. haematobium mtDNA was detected in the remaining S. haematobium × S. mattheei miracidia. From patient Y, 1 miracidium showed mixed ancestry between S. mansoni and S. mattheei, with discordance between mtDNA and nuclear DNA profiles (Appendix Figure 3). Although adult worm pairings between distantly related species usually result in the production of parthenogenetic eggs, previous experimental pairings of S. mansoni and S. mattheei resulted in the production of eggs viable to the third generation (10).
Our findings not only provide evidence of complex hybridization events in the natural setting among S. haematobium, S. mansoni, and S. mattheei but also highlight the greater relative abundance of zoonotic and hybrid schistosome species ova in feces compared with paired urine samples. That observation suggests that S. mattheei and associated hybrids, previously linked to urogenital schistosomiasis in humans, may dominate in intestinal infections by migrating to the intestinal mesenteries, just as S. mattheei likely does in other mammalian hosts where it causes rectal schistosomiasis (4). POC-CCA tests were not designed to detect zoonotic schistosomiasis; although we acknowledge that patients X and Y were both POC-CCA positive, those results do not assure the ability of POC-CCA tests to detect S. haematobium group intestinal infections because we did not perform detailed inspection of feces from POC-CCA–negative participants in the field.
In summary, we detected S. haematobium × S. mattheei hybrid ova from 2 patients in Malawi. Further fecal sampling and molecular testing with species-specific TaqMan probe assays will be essential for monitoring intestinal schistosomiasis in coendemic areas where zoonotic transmission could occur.
Dr. O’Ferrall is a clinician-scientist and PhD researcher in the Department of Tropical Disease Biology at the Liverpool School of Tropical Medicine, UK. His research focuses on the genomic epidemiology of pathogens in tropical settings, including drug-resistant bacteria and schistosomes.
We thank all participants in our study, particularly the 2 participants providing samples that enabled this analysis. We are grateful to staff and students at the Liverpool School of Tropical Medicine, Malawi-Liverpool Wellcome Programme, and Mangochi District Hospital for their valuable support and expertise in the study, including Alexandra Juhász, Sam Jones, Gladys Namacha, David Lally Jr., Priscilla Chammudzi, Donales R. Kapira, Bright Mainga, Clinton Nkolokosa, Ruth Cowlishaw, Sarah Rollason, and James E. LaCourse.
This research was funded by the National Institute for Health Research and Wellcome Trust through a Joint Investigator Award (grant no. WT 220818/Z/20/Z). A.M. O’Ferrall is supported by the Medical Research Council via the Liverpool School of Tropical Medicine-Lancaster University doctoral training partnership (grant no. MR/W007037/1).