Disclaimer: Early release articles are not considered as final versions. Any changes will be reflected in the online version in the month the article is officially released.
Author affiliation: Author affiliations: Instituto Nacional de Enfermedades Infecciosas, ANLIS “Dr. C. G. Malbrán,” Buenos Aires, Argentina (R. Paul, F. Lorenzo, B. López, N. Simboli, N.K. Yokobori); Programa de Control de Tuberculosis, Chaco, Argentina (M.G. Alegre, S. Altabe); Université des Antilles, Guadeloupe, France (D. Couvin); Institut Pasteur de Guadeloupe, Abymes, Guadeloupe (D. Couvin, N. Rastogi); Hospital General Universitario Gregorio Marañón, Madrid, Spain (L. Pérez-Lago, D. García de Viedma); Instituto de Investigaciòn Sanitaria Gregorio Marañón, Madrid (L. Pérez-Lago, D. García de Viedma); Instituto de Salud Carlos III, Madrid (D. García de Viedma); Hospital Muñiz, Buenos Aires (A. Gamberale, D. Palmero); Instituto Vaccarezza, Buenos Aires (A. Gamberale, D. Palmero); Hospital General de Niños “Pedro de Elizalde,” Buenos Aires (N. González); National Scientific and Technical Research Council, Buenos Aires (N.K. Yokobori)
Argentina is considered a mid-incidence country for tuberculosis (TB); 1% of multidrug-resistant (MDR) cases persist in Argentina. The northern province of Chaco, a province with a top 5 TB burden (1), had a low number of MDR TB cases and no prior evidence of local transmission (2). MDR TB can affect patients beyond the well-established risk groups, making clinical suspicion essential where universal drug-susceptibility testing (DST) is unavailable. Whole-genome sequencing (WGS) enables timely and precise molecular drug-resistance profiling, but genotype/phenotype correlations need further research, especially for rapidly emerging resistance to second-line drugs (e.g., bedaquiline and linezolid) (3).
To reconstruct the transmission chains and drug-resistance profiles, we used WGS to analyze an MDR TB outbreak in Resistencia, Chaco Province, Argentina. The study was performed in accordance with the Helsinki Declaration as revised in 2013. The Research Ethics Committee of the Instituto Nacional de Epidemiologia, ANLIS “Dr. Jara,” Buenos Aires, Argentina, approved the project and waived the informed consent requirement (project code YOKOBORI05/2022).
During 2018–2019, our laboratory received 9 MDR M. tuberculosis isolates from 3 patients of Resistencia, Chaco, that had unexpectedly inconsistent PCR-based resistance profiles for rifampin and isoniazid in isolates from the same patient and between 2 patients with close epidemiologic links (Appendix 1; Appendix2). A preliminary genomic analysis showed simultaneous presence of the mutations rpoB_Asp435His, rpoB_His445Asp, fabG1-inhA_t-8c, and katG_Ser315Thr. We studied that possible outbreak because of the unusual combination of mutations, the extended resistance profile, and the critical disease in young patients with no relevant comorbidities (Table 1).
The Mycobacteria Service, Instituto Nacional de Enfermedades Infecciosas, ANLIS “Dr. C. Malbrán,” Buenos Aires, Argentina, the national reference laboratory for TB diagnosis, has kept an MDR genotyping database, representing nationwide cases, since 2003. After intense screening of our databases, on the basis of rifampin and isoniazid molecular resistance patterns; province of origin; epidemiologic link, genotype, or both, we identified 29 candidate isolates from 12 patients. Twenty-four isolates were available for WGS analysis (Appendix 1); we assigned an identification number to each isolate. We performed phenotypic DST when we received the isolates unless otherwise stated (Appendixes 1, 2), and we compared spoligotypes with those in the SITVITEXTED database (Appendix 3).
All patients were residents of Resistencia, except for a patient from the neighboring Corrientes city and a former resident of Resistencia who received their diagnoses in Buenos Aires (Table 1; Appendix 3). Patient 2, a healthcare worker at the hospital where patient 1 was assisted, was the mother of patients 3, 4, and 9. Patient 6 was the granddaughter of patient 5 and frequently visited her friend, patient 10. The remaining epidemiologic links were unknown. Five patients were teenagers at the time of diagnosis (Table 1).
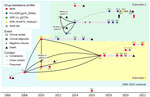
WGS showed a monophyletic group (Figure 1; Appendix 2). We named the clone the Ch strain, and it belonged to lineage 4.1.1 and to the spoligotype international type (SIT) 119 of the X1 family. The highest number of SIT119 clones in the SITVITEXTEND database in the region, without association with MDR, is in Brazil (Appendix 3). The median pairwise single-nucleotide polymorphism distance among the first isolates from each patient was 3 (range 0–6) (Appendix 2), excluding isolate 8.1, which was 15 single-nucleotide polymorphisms (range 12–17) apart from the others. The most ancestral isolate belonged to the index case-patient, whose diagnosis was made in 2006. Despite the patient having no history of TB treatment, that isolate had the 8 resistance mutations common to the cluster, including the double mutations for isoniazid and rifampin (Table 2; Figure 1), suggesting that the outbreak could have been more extended. Patient 3 was probably the source of 3 secondary pre–extensively drug-resistant cases in the second subcluster. Isolates from the patients with the most recent diagnoses (patients 11 and 12) were closer to the first subcluster (Figure 1).
The resistance mutations had high World Health Organization (WHO) confidence gradings and were concordant with the phenotypic drug-susceptibility testing results (Table 2), except for ethionamide and ethambutol, as expected (3). Resistance to the second-line injectable drugs was acquired independently in 3 isolates (Figure 1). Two isolates were extensively drug resistant. Isolate 6.4 had a rrl_g2270t mutation, which has recently been associated with linezolid resistance (3), and isolate 10.4 had the loss-of-function mutation Rv0678_144dupC. Resistance to linezolid and cross-resistance to bedaquiline were confirmed by phenotypic methods (Table 2). Instances of clofazimine/bedaquiline resistance were acquired shortly after their administration under strict supervision (Figure 2).
No compensatory mutations were found in rpoC or rpoA. Because both mutations in rpoB are expected to have a mild to high fitness cost (4), their simultaneous presence could constitute a unique compensatory mechanism.
Patient 1 died shortly after diagnosis. The mother of patient 2 had received a TB diagnosis in 2010 but refused treatment and died in 2011. The mother and the brother of patient 6 died in 2013 (Appendix 2). Isolates from those patients were not available. Because isolates 3.2, 5.1, and 6.1 were identical (Figure 1), the other 2 relatives could have acquired their infection from patient 3 (Figure 2), but their epidemiologic link remains unknown. Their close relationship, the contemporaneity, and their fatal outcomes strongly suggest that those patients were part of the outbreak (Figure 2). Patient 9 probably experienced relapse from latency and infected patient 12, who lived at the same address before moving to Buenos Aires. Their relationship remains unclear. Patient 2 administered the medication to her family, including the injectable drugs. Some regimens, especially in the first years of the outbreak, were suboptimal and underwent multiple changes. Reports suggest that empathy from some healthcare providers had been insufficient. Three cohabitants received chemoprophylaxis with isoniazid, and no active disease has been reported (Appendix 2).
The MDR Ch outbreak strain, with its epicenter in Resistencia, Chaco, belonged to the X1, SIT 119 spoligotype, which is infrequent in Argentina (5,6) (Appendix 3). The X family has been associated with high transmissibility (7,8), and SIT119 could have been imported from Brazil, considering the frequent cross-border movements to and from Chaco (Appendix 3). Further phylogenomic studies are warranted to determine the precise origin of that MDR strain.
Several factors converged in the outbreak. It started as intrahospital transmission to a healthcare worker, who spread the disease to her cohabitants (Figure 2). Despite her background, the family was poorly receptive to and not compliant with treatment. On other hand, some healthcare workers were not appropriately prepared to manage MDR TB. Delayed diagnosis, poor compliance, and administration of suboptimal regimens led to long periods of culture positivity, amplification of resistance, and an alarmingly high mortality rate (53%). In addition to lack of effective drugs, host and bacterial genetic factors could have played a role. Several patients were relatives, which suggests genetic susceptibility to TB. Conversely, the observed mortality rate suggests higher virulence of the Ch strain. Although challenging to assess their relative effect, those biological and societal factors collectively shaped the outbreak outcome.
We gained valuable insights from our study. The phylogenetic analysis strongly suggests additional missing cases, and although no new cases were diagnosed, MDR TB surveillance in Chaco must be strengthened. Of note, Ch genotype can be suspected by detecting the rpoB double mutation through GeneXpert and other molecular tests (data not shown). Next-generation tools, including novel drugs and WGS, are available, but clinical suspicion of MDR-TB remains crucial for their effective use. Continuing education and active engagement of healthcare professionals and the community are vital for managing future outbreaks.
Mrs. Paul is a professional of the Servicio de Micobacterias, INEI, ANLIS “C. G. Malbrán” and the Hospital Piñero, Buenos Aires, Argentina, with a research interest in the microbiological diagnosis of mycobacterial diseases.